Front-line physicians at Edmonton's Royal Alexandra Hospital report that provincial pilot projects aimed at alleviating severe emergency department congestion have yet to produce meaningful improvements, describing the initiatives as "glorified experiments."
Pilot Projects in Place, But Results Lag
The Alberta government has implemented several test programs at the busy Edmonton hospital, which experiences some of the highest patient volumes and complexity in the province. These initiatives, which began rolling out in September 2025, include deploying social workers in the ER around the clock, seconding nurse practitioners from other areas to assist emergency doctors, redistributing internal medicine cases to other sites, and transferring alternative level of care (ALC) patients out of the hospital to other settings.
The province's Ministry of Hospitals and Surgical Health Services has stated the Royal Alex is an "ideal site to test solutions" to improve patient flow and reduce ER pressures before potentially expanding the projects across Alberta.
Front-Line Staff See "No Dramatic Difference"
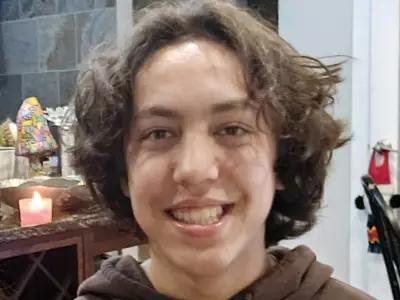
Despite these measures, doctors working in the trenches say the situation remains dire. Dr. Warren Thirsk, head of emergency medicine for the Alberta Medical Association and an ER physician at the Royal Alex, is blunt in his assessment.
"The front line has not noticed any dramatic differences because these pilot projects, as they like to label them, are really just glorified experiments and they have not made a big difference," Dr. Thirsk told Postmedia.
He explained that efforts to move admitted patients out of emergency beds and into hospital wards upstairs have been consistently "derailed" by other systemic failures within the hospital. The fundamental issue, he stresses, is a fixed number of beds compounded by a faltering broader system.
Waiting Rooms Routinely Packed with Dozens
The tangible impact of the ongoing crisis is felt daily by patients. Dr. Thirsk reports that the ER's waiting room routinely holds 50 patients, with peaks exceeding 100 patients at one time. He notes he has yet to witness a day where the waiting room has fewer than 30 people awaiting care.
"We have 30 or more (patients) leaving every day who just get tired of the wait," Thirsk said, drawing a stark contrast with other sectors. "When we have these type of waits or backlogs happen in airports, there's federal policy and quick rules and things are changed. When we have it in health care, we just shrug our shoulders."
One recent measure involves using nurse practitioners to take over some duties from emergency physicians, theoretically freeing doctors to see more patients. While Thirsk acknowledges this might offer slight relief for night doctor burnout, he is skeptical it will address the core problem.
"It's not going to make a significant difference to our waiting rooms or to anything else because we have a fixed number of beds, and with these other parts of the system faltering, these initiatives don't make a difference," he concluded.
As the province hopes to scale these pilot projects, the feedback from the hospital's front line suggests that without addressing fundamental capacity and flow issues, emergency room gridlock at the Royal Alexandra Hospital is likely to persist.