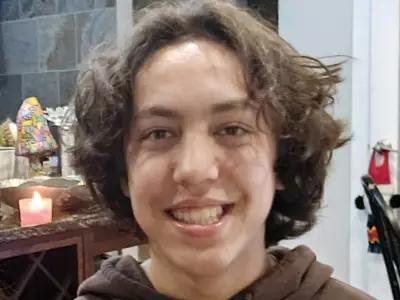
The death of a 44-year-old father after an eight-hour wait in an Edmonton emergency room has cast a stark and tragic light on the deepening crisis within Alberta's healthcare system. Prashant Sreekumar, a father of two, died in the waiting room of the Grey Nuns Community Hospital, an event that has devastated his family and traumatized the healthcare workers on duty that day.
A Symptom of Systemic Collapse
While it is easy to point fingers at triage protocols or the emergency department (ED) itself, experts argue this tragedy is the result of a far broader system failure. The ED has become the catch-all for every crack in Alberta's healthcare foundation. Although a shortage of family doctors sends many to emergency, fixing primary care access alone will not solve the critical overcrowding problem.
The demand is surging from all directions. Patients facing intolerable delays for specialist appointments, CT scans, and MRIs are turning to emergency rooms to expedite care or because their symptoms have become unmanageable. An aging population with more complex, chronic illnesses and a surge in unmet mental health needs are further overwhelming emergency departments.
The Root of the Gridlock: What Happens After the ER
The core issue fueling emergency room gridlock often begins after a patient is seen. In major centres like Calgary and Edmonton, it is now routine for over half of all ED beds to be occupied by patients who have been admitted to the hospital but are waiting for a bed to open up upstairs. Hospital capacity routinely exceeds 100%, partly because nearly a quarter of usable acute care beds are blocked by patients who should be in continuing care. In some Edmonton hospitals recently, that figure spiked to 40%.
This persistent problem has been magnified by low vaccination rates for COVID-19 and influenza, a situation public health experts link to the provincial government's stance on vaccinations. This has led to hospitals being overwhelmed with preventable respiratory virus cases.
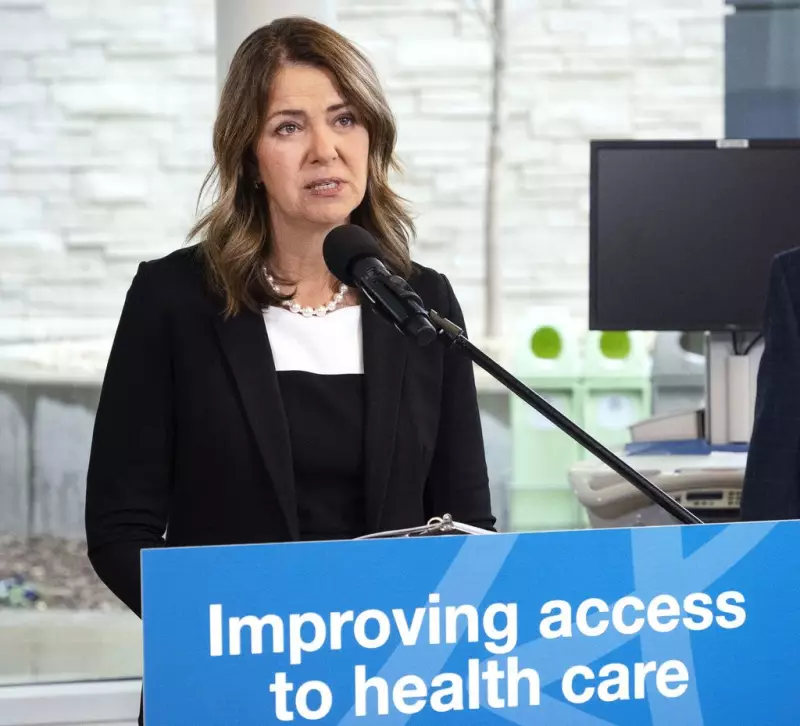
A Broken Promise on a "Seamless" System
These systemic failures are not new. In September 2024, amid growing concerns that the government's plan to break Alberta Health Services into four separate agencies would create further chaos, the province commissioned a report from former health minister Dr. Lyle Oberg. The government launched the Seamless Patient Experience Review, with a report due in March 2025, promising better integration.
True healthcare integration—where patients, especially the elderly or those with chronic diseases, move smoothly between different levels of care—remains essential. It is also critically important for seemingly healthy individuals like Prashant Sreekumar, who needed immediate, safe emergency care but could not receive it because the system was gridlocked.
The tragic death at the Grey Nuns Hospital stands as a sombre indictment of the current state of affairs, raising urgent and unresolved questions about the government's ability to deliver on its promised vision for patient care.