The tragic stories of two Canadian men who died after enduring agonizing waits in hospital emergency departments have become grim symbols of a national healthcare system in crisis. Their cases highlight a fatal flaw that many within the system whisper about but few address publicly: the draining of clinical staff into administrative roles.
A Haunting Pattern of Neglect
In early 2026, the death of Prashant Sreekumar, a 44-year-old Edmonton father, shocked the nation. He waited over eight hours in an emergency department while suffering chest pain, only to succumb without receiving the urgent care he needed. A devastating video circulated showing his wife confronting hospital staff beside his body on a stretcher.
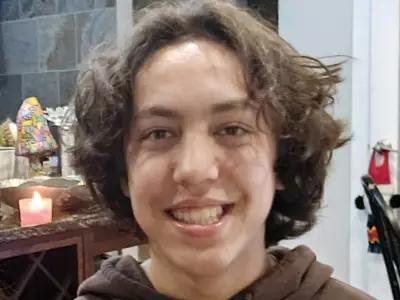
His case bore a chilling resemblance to that of Adam Burgoyne, 39, who died in December 2024. After waiting for hours with chest pain at a Montreal hospital, Burgoyne left in frustration. He posted a final, sardonic message on social media: "Had a bit of a health scare last night... once they made sure I wasn't dying I was thrown out into the waiting room and 6 hours later I said f*ck it and went home. Canadian health care, folks. Best in the world." He was dead the next day from an aortic dissection.
Both men received initial ECGs upon arrival but were then relegated to the waiting room. A subsequent coroner's report confirmed the hospital erred in not prioritizing Burgoyne's case. Even entrepreneur Elon Musk commented on the tragedy, noting the fragility of life. Yet, as author and former healthcare worker Amy Hamm points out, no systemic changes followed Burgoyne's death. A year later, Sreekumar met the same fate.
The Real Culprit: A Bloated Bureaucracy
While public discourse often rightly deflects blame from overworked nurses and doctors, Hamm argues this has become a platitude that shields the truly responsible parties. Drawing on over a decade of experience within public healthcare, she identifies a critical and growing problem: the migration of licensed care providers from the front lines to administrative roles.
"I witnessed the administrative and bureaucratic class fatten up over this time," Hamm writes. She observed dozens of skilled clinicians—people trained for hands-on patient care—being pulled into management, middle management, special projects, and accreditation roles. These positions often offer better hours, less stress, and higher pay than the grueling work in emergency departments or on hospital wards.
A Call for Administrative Staff to Return to Care
The solution, Hamm contends, is not simply more funding or vague promises of reform. It requires a fundamental re-prioritization of human resources within the system. Healthcare bureaucrats with clinical credentials need to return to the front lines. Their skills are desperately needed where patients are dying in waiting rooms.
This exodus of talent from clinical care to paperwork has created a dangerous vacuum at the point of greatest need. The result is a fatality-prone medical crisis where triage systems fail and patients with critical conditions are not seen in time. The deaths of Burgoyne and Sreekumar are not isolated incidents but symptoms of a structural imbalance that values administration over direct patient intervention.
Until healthcare leaders address this internal drain and incentivize skilled professionals to remain in or return to clinical roles, Canadians will continue to be at risk. The promise of universal healthcare is broken not at the policy level, but in the overcrowded waiting rooms where the system's human resource failures become matters of life and death.