Taylor Coffman lay in her hospital bed, struggling to answer simple questions from her internist. The date was February 17, 2022, and she knew President Biden led the country, but each response came with tremendous difficulty. Her arms twitched uncontrollably, rendering them practically useless.
A Medical Nightmare Begins
Four weeks earlier, Taylor had given birth to her daughter via C-section. Instead of the joyful moment new mothers anticipate, chaos erupted immediately after delivery. Her vitals plummeted and she began bleeding out rapidly, requiring emergency surgery before she even had the chance to hold her newborn. She didn't wake from the anesthesia right away, beginning what would become a living nightmare.
When Taylor finally regained consciousness four days later, she met her daughter briefly before the baby went home without her. Thus began a grueling hospital stay that would see her cycling in and out of the ICU multiple times. Her husband Zach received the dreaded middle-of-the-night call that she might not survive.
Doctors struggled to identify what was wrong with Taylor as her body systems failed one after another. She endured three rounds of ICU intubation, multiple abdominal surgeries, blood clots throughout her body, heart failure, kidney failure, severe sepsis, and pneumonia. She describes herself during this period as a forever-changed, half-dead person.
Becoming Her Own Project Manager
Once finally removed from the ventilator for the last time, Taylor discovered a frustrating reality: her numerous specialists often gave conflicting information about her condition. With backgrounds including work at Jimmy Kimmel Live and NPR station KPCC, she brought her professional project management skills to her medical crisis.
I'm a project manager at my day job, and you all have got to get organized working across fields, she told one physician. In response to her advocacy, her doctors created a text chain to improve communication between the fetal maternal medicine team, cardiologist, hematologist, nephrologist, infectious disease specialist, pulmonologist, and surgical team.
That simple text chain might have saved her life, and it likely wouldn't have happened without Taylor speaking up. This realization marked a turning point in her approach to her care.
The Power of Patient Advocacy
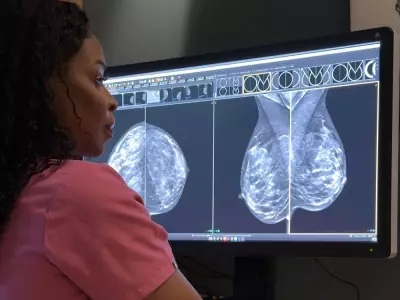
Taylor's hematologist suspected she had atypical hemolytic uremic syndrome (aHUS), an extremely rare disease that often remains dormant until triggered by pregnancy. The condition is particularly dangerous and claims many lives.
Despite sharing concerning new symptoms with her medical team, including increasing shakes and stutters, Taylor felt dismissed. Her internist suggested medication side effects, while other doctors recommended anti-anxiety medication. Hours later, she experienced terrifying symptoms where everything in her perception repeated three times, followed by complete loss of speech.
Her body was poisoning her brain with toxins because her kidneys were failing. She desperately needed dialysis, but no machines were available at the massive, cutting-edge hospital. Taylor had reached the point of toxic encephalopathy, experiencing aphasia and nervous system tremors.
The data supports Taylor's experience of being dismissed. A 2009 study showed middle-aged women with the same heart disease symptoms as men were twice as likely to be diagnosed with a mental health issue. The Journal of American Heart Association found women possibly experiencing heart attacks wait 29% longer in ERs than men.
Recent CDC data indicates 1 in 5 women experience mistreatment during pregnancy, with significantly worse statistics for Black women contributing to higher maternal mortality rates.
Lessons for All Patients
Five grueling weeks after giving birth, Taylor finally went home to her baby. Her hematologist's theory proved correct - she indeed had aHUS. After nine months of dialysis, her kidney regained some function, leaving her with stage 3 kidney disease.
Today, Taylor manages her chronic rare disease with infusions every eight weeks and embraces being a mom to her active toddler. She approaches healthcare differently now, recognizing that while doctors have medical expertise, she remains the expert on herself.
Her current strategies include organizing bullet points of symptoms in her phone's notes app, doing thorough research before appointments, asking doctors to annotate her chart when they decline requested tests, and sometimes recording conversations to ensure she doesn't miss important information.
Most people don't want to be a squeaky wheel, but be a squeaky wheel, Taylor advises. Research confirms that empowered patients often experience better health outcomes. She maintains respect and kindness while being insistent about her care.
Taylor's journey through maternal medical crisis taught her the vital importance of advocating for her needs and trusting herself when something feels wrong. Her experience demonstrates how patient empowerment can literally mean the difference between life and death.